When we discuss diabetes, the conversation typically revolves around blood sugar management and its impact on overall health. However, what often goes unnoticed is the profound effect diabetes can have on oral health, particularly concerning teeth, bone density, and gum tissue. Delving into this connection is vital for both patients and healthcare professionals to comprehend the risks involved and implement effective preventive measures.
Unveiling the Link: Diabetes, whether type 1 or type 2, disrupts the body’s ability to regulate blood sugar levels efficiently. This chronic elevation in blood glucose can trigger a series of adverse effects throughout the body, including the oral cavity, which can significantly affect teeth health.
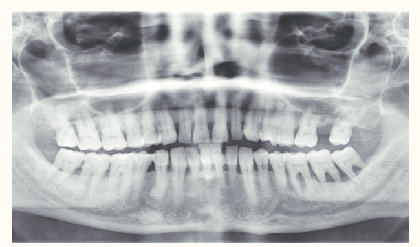
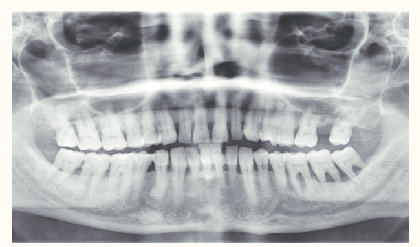
Bone Loss: Research indicates a clear correlation between uncontrolled diabetes and reduced bone density. Elevated blood sugar levels can impede the body’s capacity to generate new bone tissue and hinder the repair of existing bone. Consequently, individuals with diabetes may experience a condition known as osteoporosis, characterized by weakened bones that are prone to fractures.
Gum Recession: In addition to bone loss, uncontrolled diabetes can contribute to gum recession, where the gum tissue pulls away from the teeth, exposing their roots. This gradual and often painless process can go unnoticed until significant damage has occurred. Gum recession not only compromises the aesthetics of the smile but also increases the risk of tooth decay, sensitivity, and ultimately, tooth loss.
The Dangers: The ramifications of bone loss and gum recession extend beyond the oral cavity, significantly impacting dental health and overall well-being for individuals with diabetes:
- Tooth Loss: Weakened bone support and receding gums can lead to loosening and eventual loss of teeth.
- Periodontal Disease: Gum recession creates pockets where bacteria thrive, increasing the risk of gum disease, a severe infection associated with tooth loss and systemic health complications.
- Impaired Healing: Poor bone density and compromised gum tissue can hinder the body’s ability to heal following dental procedures or injuries.
- Jawbone Infections: Severe bone loss can leave the jaw vulnerable to infections, necessitating extensive treatment or surgical intervention.
Treatment and Prevention: Thankfully, proactive management of diabetes and stringent oral hygiene practices can help mitigate the risks associated with bone loss and gum recession, safeguarding teeth and overall oral health:
- Blood Sugar Control: Maintaining blood glucose levels within target ranges through medication, diet, and exercise is crucial for preventing further damage to bone and gum tissue.
- Regular Dental Checkups: Routine dental exams enable early detection and treatment of oral health issues before they escalate.
- Proper Oral Hygiene: Consistent brushing, flossing, and using antibacterial mouthwash can prevent plaque buildup and gum disease.
- Lifestyle Modifications: Avoiding tobacco use and consuming a balanced diet rich in calcium and vitamin D can support oral and bone health.
- Professional Intervention: In cases of existing bone loss or gum recession, dental treatments like bone grafting, gum grafting, or periodontal therapy may be necessary to restore oral health and function.
Understanding the intricate connection between diabetes and teeth health is paramount for effectively managing the condition and preventing dental complications. By prioritizing blood sugar control, maintaining diligent oral hygiene, and seeking timely professional intervention, individuals can safeguard their teeth and overall oral well-being, enhancing their quality of life despite living with diabetes. Collaboration between patients, healthcare providers, and dental professionals is essential in addressing this critical aspect of diabetes management and ensuring optimal dental health outcomes.
Contact Us to discuss your dental health.